Anemia
| Anemia | |
|---|---|
|
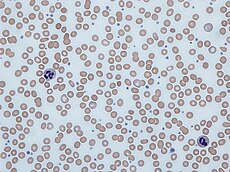
Human blood from a case of iron-deficiency anemia
|
|
Anemia, also spelled anaemia, is usually defined as a decrease in the amount of red blood cells (RBCs) or hemoglobin in the blood.[1][2] It can also be defined as a lowered ability of the blood to carry oxygen.[3] When anemia comes on slowly the symptoms are often vague and may include: feeling tired, weakness, shortness of breath or a poor ability to exercise. Anemia that comes on quickly often has greater symptoms which may include: confusion, feeling like one is going to pass out, loss of consciousness, or increased thirst. Anemia must be significant before a person becomes noticeably pale. Additional symptoms may occur depending on the underlying cause.[4]
There are three main types of anemia: that due to blood loss, that due to decreased red blood cell production, and that due to increased red blood cell breakdown. Causes of blood loss include trauma and gastrointestinal bleeding, among others. Causes of decreased production include iron deficiency, a lack of vitamin B12, thalassemia and a number of neoplasms of the bone marrow among others. Causes of increased breakdown include a number of genetic conditions such as sickle cell anemia, infections like malaria and some autoimmune diseases among others. It can also be classified based on the size of red blood cells and amount of hemoglobin in each cell. If the cells are small it is microcytic anemia, if they are large it is macrocytic anemia and if they are normal sized it is normocytic anemia. Diagnosis in men is based on a hemoglobin of less than 130 to 140 g/L (13 to 14 g/dL), while in women it must be less than 120 to 130 g/L (12 to 13 g/dL).[4][5] Further testing is then required to determine the cause.[4]
Certain groups of individuals, such as pregnant women, benefit from the use of iron pills for prevention.[4][6] Dietary supplementation, without determining the specific cause, is not recommended. The use of blood transfusions is typically based on a person's signs and symptoms.[4] In those without symptoms they are not recommended unless hemoglobin levels are less than 60 to 80 g/L (6 to 8 g/dL).[4][7] These recommendations may also apply to some people with acute bleeding.[4] Erythropoiesis-stimulating medications are only recommended in those with severe anemia.[7]
Anemia is the most common disorder of the blood with it affecting about a quarter of people globally.[4] Iron-deficiency anemia affects nearly 1 billion.[8] In 2013 anemia due to iron deficiency resulted in about 183,000 deaths – down from 213,000 deaths in 1990.[9] It is more common in females than males,[8] among children, during pregnancy, and in the elderly.[4] Anemia increases costs of medical care and lowers a person's productivity through a decreased ability to work.[5] The name is derived from Ancient Greek: ἀναιμία anaimia, meaning "lack of blood", from ἀν- an-, "not" + αἷμα haima, "blood".[10]
Contents
Signs and symptoms
Main symptoms that may appear in anemia[11]
Causes
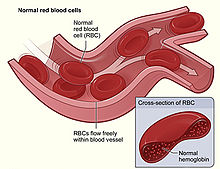
Figure shows normal red blood cells flowing freely in a blood vessel.
The inset image shows a cross-section of a normal red blood cell with
normal hemoglobin.[12]
Impaired production
- Disturbance of proliferation and differentiation of stem cells
- Pure red cell aplasia[14]
- Aplastic anemia[14] affects all kinds of blood cells. Fanconi anemia is a hereditary disorder or defect featuring aplastic anemia and various other abnormalities.
- Anemia of renal failure[14] by insufficient erythropoietin production
- Anemia of endocrine disorders[medical citation needed]
- Disturbance of proliferation and maturation of erythroblasts
- Pernicious anemia[14] is a form of megaloblastic anemia due to vitamin B12 deficiency dependent on impaired absorption of vitamin B12. Lack of dietary B12 causes non-pernicious megaloblastic anemia
- Anemia of folic acid deficiency,[14] as with vitamin B12, causes megaloblastic anemia
- Anemia of prematurity, by diminished erythropoietin response to declining hematocrit levels, combined with blood loss from laboratory testing, generally occurs in premature infants at two to six weeks of age.
- Iron deficiency anemia, resulting in deficient heme synthesis[14]
- Thalassemias, causing deficient globin synthesis[14]
- Congenital dyserythropoietic anemias, causing ineffective erythropoiesis
- Anemia of renal failure[14] (also causing stem cell dysfunction)
- Other mechanisms of impaired RBC production
- Myelophthisic anemia[14] or myelophthisis is a severe type of anemia resulting from the replacement of bone marrow by other materials, such as malignant tumors or granulomas.
- Myelodysplastic syndrome[14]
- anemia of chronic inflammation[14]
Increased destruction
Further information: Hemolytic anemia
Anemias of increased red blood cell destruction are generally classified as hemolytic anemias. These are generally featuring jaundice and elevated lactate dehydrogenase levels.[medical citation needed]- Intrinsic (intracorpuscular) abnormalities[14] cause premature destruction. All of these, except paroxysmal nocturnal hemoglobinuria, are hereditary genetic disorders.[15]
- Hereditary spherocytosis[14] is a hereditary defect that results in defects in the RBC cell membrane, causing the erythrocytes to be sequestered and destroyed by the spleen.
- Hereditary elliptocytosis[14] is another defect in membrane skeleton proteins.
- Abetalipoproteinemia,[14] causing defects in membrane lipids
- Enzyme deficiencies
- Pyruvate kinase and hexokinase deficiencies,[14] causing defect glycolysis
- Glucose-6-phosphate dehydrogenase deficiency and glutathione synthetase deficiency,[14] causing increased oxidative stress
- Hemoglobinopathies
- Sickle cell anemia[14]
- Hemoglobinopathies causing unstable hemoglobins[14]
- Paroxysmal nocturnal hemoglobinuria[14]
- Extrinsic (extracorpuscular) abnormalities
- Antibody-mediated
- Warm autoimmune hemolytic anemia is caused by autoimmune attack against red blood cells, primarily by IgG. It is the most common of the autoimmune hemolytic diseases.[16] It can be idiopathic, that is, without any known cause, drug-associated or secondary to another disease such as systemic lupus erythematosus, or a malignancy, such as chronic lymphocytic leukemia.[17][17]
- Cold agglutinin hemolytic anemia is primarily mediated by IgM. It can be idiopathic[18] or result from an underlying condition.
- Rh disease,[14] one of the causes of hemolytic disease of the newborn
- Transfusion reaction to blood transfusions[14]
- Mechanical trauma to red cells
- Antibody-mediated
Blood loss
- Anemia of prematurity from frequent blood sampling for laboratory testing, combined with insufficient RBC production
- Trauma[14] or surgery, causing acute blood loss
- Gastrointestinal tract lesions,[14] causing either acute bleeds (e.g. variceal lesions, peptic ulcers or chronic blood loss (e.g. angiodysplasia)
- Gynecologic disturbances,[14] also generally causing chronic blood loss
- From menstruation, mostly among young women or older women who have fibroids
- Infection by intestinal nematodes feeding on blood, such as hookworms[19] and the whipworm Trichuris trichiura.[20]
Fluid overload
Fluid overload (hypervolemia) causes decreased hemoglobin concentration and apparent anemia:- General causes of hypervolemia include excessive sodium or fluid intake, sodium or water retention and fluid shift into the intravascular space.[21]
- Anemia of pregnancy is induced by blood volume expansion experienced in pregnancy.[medical citation needed]
Diagnosis
Peripheral blood smear microscopy of a patient with iron-deficiency anemia
In modern counters, four parameters (RBC count, hemoglobin concentration, MCV and RDW) are measured, allowing others (hematocrit, MCH and MCHC) to be calculated, and compared to values adjusted for age and sex. Some counters estimate hematocrit from direct measurements.[medical citation needed]
| Age or gender group | Hb threshold (g/dl) | Hb threshold (mmol/l) |
|---|---|---|
| Children (0.5–5.0 yrs) | 11.0 | 6.8 |
| Children (5–12 yrs) | 11.5 | 7.1 |
| Teens (12–15 yrs) | 12.0 | 7.4 |
| Women, non-pregnant (>15yrs) | 12.0 | 7.4 |
| Women, pregnant | 11.0 | 6.8 |
| Men (>15yrs) | 13.0 | 8.1 |
Red blood cell size
In the morphological approach, anemia is classified by the size of red blood cells; this is either done automatically or on microscopic examination of a peripheral blood smear. The size is reflected in the mean corpuscular volume (MCV). If the cells are smaller than normal (under 80 fl), the anemia is said to be microcytic; if they are normal size (80–100 fl), normocytic; and if they are larger than normal (over 100 fl), the anemia is classified as macrocytic. This scheme quickly exposes some of the most common causes of anemia; for instance, a microcytic anemia is often the result of iron deficiency. In clinical workup, the MCV will be one of the first pieces of information available, so even among clinicians who consider the "kinetic" approach more useful philosophically, morphology will remain an important element of classification and diagnosis. Limitations of MCV include cases where the underlying cause is due to a combination of factors - such as iron deficiency (a cause of microcytosis) and vitamin B12 deficiency (a cause of macrocytosis) where the net result can be normocytic cells.[medical citation needed]Production vs. destruction or loss
The "kinetic" approach to anemia yields arguably the most clinically relevant classification of anemia. This classification depends on evaluation of several hematological parameters, particularly the blood reticulocyte (precursor of mature RBCs) count. This then yields the classification of defects by decreased RBC production versus increased RBC destruction and/or loss. Clinical signs of loss or destruction include abnormal peripheral blood smear with signs of hemolysis; elevated LDH suggesting cell destruction; or clinical signs of bleeding, such as guaiac-positive stool, radiographic findings, or frank bleeding.[medical citation needed] The following is a simplified schematic of this approach:[medical citation needed]* For instance, sickle cell anemia with superimposed iron deficiency; chronic gastric bleeding with B12 and folate deficiency; and other instances of anemia with more than one cause.
** Confirm by repeating reticulocyte count: ongoing combination of low reticulocyte production index, normal MCV and hemolysis or loss may be seen in bone marrow failure or anemia of chronic disease, with superimposed or related hemolysis or blood loss. Here is a schematic representation of how to consider anemia with MCV as the starting point:
|
|
|
|
|
|
|
|
|
Anemia |
|
|
|
|
|
|
|||||||||||||||||||||||||||||||
|
|
|
|
|
|
Reticulocyte production index shows inadequate production response to anemia. |
|
|
|
Reticulocyte production index shows appropriate response to anemia = ongoing hemolysis or blood loss without RBC production problem. |
|
|
|
|||||||||||||||||||||||||||||||||
|
|
No clinical findings consistent with hemolysis or blood loss: pure disorder of production. |
|
Clinical findings and abnormal MCV: hemolysis or loss and chronic disorder of production*. |
|
Clinical findings and normal MCV= acute hemolysis or loss without adequate time for bone marrow production to compensate**. |
|
|||||||||||||||||||||||||||||||||||||||
|
|
Macrocytic anemia (MCV>100) |
|
Normocytic anemia (80|
|
|
Microcytic anemia (MCV<80 td="">
|
|
|
|
|
| |||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
Anemia |
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||
|
|
|
|
Macrocytic anemia (MCV>100) |
|
|
|
|
|
Normocytic anemia (MCV 80–100) |
|
|
|
|
|
Microcytic anemia (MCV<80 td=""> | ||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
High reticulocyte count |
|
|
|
|
|
Low reticulocyte count |
|
|
|
|
||||||||||||||||||||||||||||
Other characteristics visible on the peripheral smear may provide valuable clues about a more specific diagnosis; for example, abnormal white blood cells may point to a cause in the bone marrow.
Microcytic
Main article: Microcytic anemia
Microcytic anemia is primarily a result of hemoglobin synthesis
failure/insufficiency, which could be caused by several etiologies:- Heme synthesis defect
- Iron deficiency anemia (microcytosis is not always present)
- Anemia of chronic disease (more commonly presenting as normocytic anemia)
- Globin synthesis defect
- Alpha-, and beta-thalassemia
- HbE syndrome
- HbC syndrome
- Various other unstable hemoglobin diseases
- Sideroblastic defect
- Hereditary sideroblastic anemia
- Acquired sideroblastic anemia, including lead toxicity
- Reversible sideroblastic anemia
- Iron deficiency anemia is due to insufficient dietary intake or absorption of iron to meet the body's needs. Infants, toddlers, and pregnant women have higher than average needs. Increased iron intake is also needed to offset blood losses due to digestive tract issues, frequent blood donations, or heavy menstrual periods.[23] Iron is an essential part of hemoglobin, and low iron levels result in decreased incorporation of hemoglobin into red blood cells. In the United States, 12% of all women of childbearing age have iron deficiency, compared with only 2% of adult men. The incidence is as high as 20% among African American and Mexican American women.[24] Studies have shown iron deficiency without anemia causes poor school performance and lower IQ in teenage girls, although this may be due to socioeconomic factors.[25][26] Iron deficiency is the most prevalent deficiency state on a worldwide basis. It is sometimes the cause of abnormal fissuring of the angular (corner) sections of the lips (angular stomatitis).
- In the United States, the most common cause of iron deficiency is bleeding or blood loss, usually from the gastrointestinal tract. Fecal occult blood testing, upper endoscopy and lower endoscopy should be performed to identify bleeding lesions. In older men and women, the chances are higher that bleeding from the gastrointestinal tract could be due to colon polyps or colorectal cancer.
- Worldwide, the most common cause of iron deficiency anemia is parasitic infestation (hookworms, amebiasis, schistosomiasis and whipworms).[27]
Macrocytic
Main article: Macrocytic anemia
- Megaloblastic anemia, the most common cause of macrocytic anemia, is due to a deficiency of either vitamin B12, folic acid, or both. Deficiency in folate and/or vitamin B12 can be due either to inadequate intake or insufficient absorption. Folate deficiency normally does not produce neurological symptoms, while B12 deficiency does.
- Pernicious anemia is caused by a lack of intrinsic factor, which is required to absorb vitamin B12 from food. A lack of intrinsic factor may arise from an autoimmune condition targeting the parietal cells (atrophic gastritis) that produce intrinsic factor or against intrinsic factor itself. These lead to poor absorption of vitamin B12.
- Macrocytic anemia can also be caused by removal of the functional portion of the stomach, such as during gastric bypass surgery, leading to reduced vitamin B12/folate absorption. Therefore, one must always be aware of anemia following this procedure.
- Hypothyroidism
- Alcoholism commonly causes a macrocytosis, although not specifically anemia. Other types of liver disease can also cause macrocytosis.
- Drugs such as Methotrexate, zidovudine, and other substances may inhibit DNA replication such as heavy metals (e.g. Lead)
Normocytic
Main article: Normocytic anemia
Normocytic anemia occurs when the overall hemoglobin levels are decreased, but the red blood cell size (mean corpuscular volume) remains normal. Causes include:- Acute blood loss
- Anemia of chronic disease
- Aplastic anemia (bone marrow failure)
- Hemolytic anemia



No comments:
Post a Comment